Breaking Ebola transmission chains
Interview with
Although media coverage has decreased, the Ebola crisis that dominated the news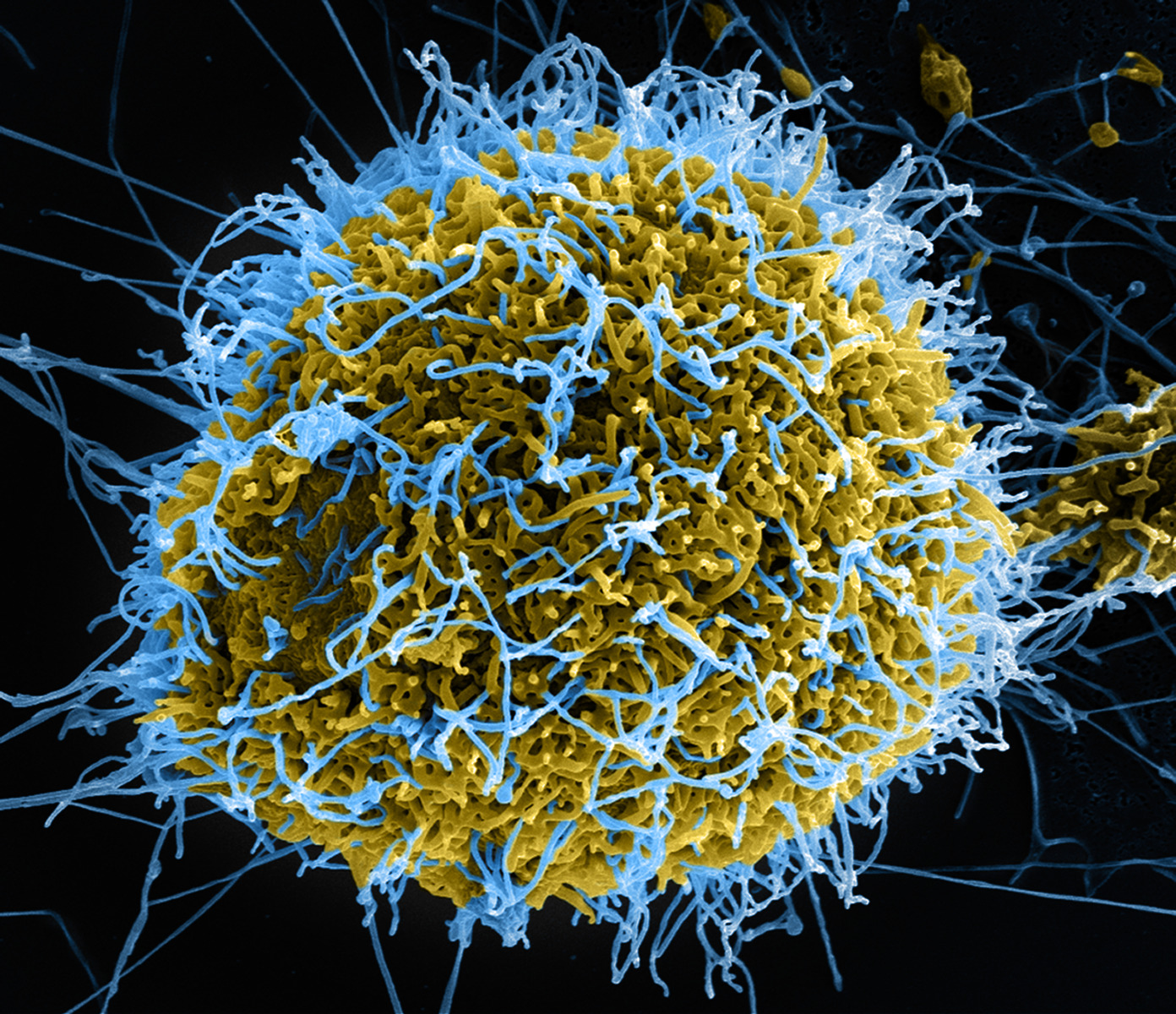 across much of last year hasn't actually ended and there are still cases being declared. Now scientists have a new weapon to break the so called transmission chain of ebola and that's a DNA sequencer. Cambridge virologist Ian Goodfellow has been in Sierra Leone where he's installed this machine - in a tent - and it's reading the genetic information of viruses recovered from victims, enabling scientists - and the government locally - to act more effectively. The first publicly-available data came off the machine this week. Previously, getting samples to analyse like this, was nearly impossible, as he explained to Chris Smith...
across much of last year hasn't actually ended and there are still cases being declared. Now scientists have a new weapon to break the so called transmission chain of ebola and that's a DNA sequencer. Cambridge virologist Ian Goodfellow has been in Sierra Leone where he's installed this machine - in a tent - and it's reading the genetic information of viruses recovered from victims, enabling scientists - and the government locally - to act more effectively. The first publicly-available data came off the machine this week. Previously, getting samples to analyse like this, was nearly impossible, as he explained to Chris Smith...
Ian - You have to get this material out of the country and you have two options. One is you take the actual infectious material out which has real challenges because the commercial flights won't carry it. Or you take the genetic material out and that has its other challenges because you need to be confident that you're inactivating the material. So, just the practicalities of getting the samples that have come out of the patients and physically getting them out of the country, getting permissions means that the whole process is slowed down.
Chris - So, how did you seek to address this?
Ian - The aim is really to try and put a machine that would allow us to determine the genetic sequence of these viruses in a treatment centre in Makeni. This is in Bombali District in Sierra Leone, in what really can only be described as a rather unconventional environment.
Chris - Just describe first of all, what do these machines that read genetic information look like?
Ian - It's probably the size of a reasonable-sized television, like a big box effectively. It just looks like a box with a whole bunch of tubes coming out of it. The machine we chose, we selected for a very specific reason and that was because we felt we could operate it in that environment. We needed something that's going to be able to cope with the temperature, cope with the humidity, cope with the dust, the insects that are crawling around the inside of the tent.
Chris - And the data is now coming off of the machine is it? You're getting sequences now from this machine.
Ian - We are getting sequences. One of the big problems we faced is getting the data out. Here in the UK, I have a superfast broadband which means I can send large files across from here anywhere in the world very, very quickly. In Sierra Leone, we're trying to move somewhere in the region of 5 gigabytes of data per run of the machine. We're doing this on a Wi-Fi dongle, so this is slower than the internet connection you will get from a mobile phone.
Chris - But critically, this means that now, you're literally testing the genetic sequence of Ebola that is infecting people and you can therefore marry up what the outcome was for that person where they'd come from in a country who they'd had contact with and perhaps whether or not those viruses spread. I presume you can begin to learn something about how the viruses behave based on their genetic information and how fast they're changing and so on.
Ian - The only way to be able to break transmission chains is if you know how that transmission chain is operating and there's clear evidence from the sequences we've released already that there's numerous viruses coming in from numerous examples of infected individuals getting viruses from Guinea. So, we're finding viruses in Sierra Leone that actually come from Guinea. That's despite the border being closed. Officially, that border is closed and there should be no movement of individuals across the border. But they're very porous borders and they're difficult to police. So, this gives you an indication that there is multiple incursions of Guinean viruses into Sierra Leone. This is something we need to be aware of and there are things that could be done on the ground with that information.
Chris - So, by reading the genetic information, you're actually learning quite a bit about what's happening politically or geographically in a country as well, aren't you?
Ian - We can, yeah absolutely. You can see our data would indicate that there's at least 12 independent transmission chains which are operating. Now, actually the government has done a fantastic job and many of those transmission chains we think are stopped. But if we see new cases appearing and anywhere in the country, we have a system set up now where the laboratory will phone the sequencing facility and we will go and collect that sample within 24 hours and sequence it. So, our plan is to make the sequences publicly available as fast as possible. We feel that it's important that this information is freely distributed to anyone who wants to see it or anyone who can analyse it because only by really opening up that data can you draw on the wealth of knowledge of people who are not able to actually go in country to do that sort of analysis. We can provide them with that data and they can use their expertise to analyse it. That analysis is then fed back to the public health people on the ground.
Chris - Is this the first time to your knowledge that somebody has put a sequencer that reads genetic data into a tent in an African country, not just for Ebola but for anything really and really broken this bottleneck like this?
Ian - I would hesitate to say that we're the first to do this. I'm not aware myself of anybody else with a sequencer that is on the ground. One thing we've learned from this outbreak, it's taken us 5 months to get to this point and that's too slow. We need the ability to have this equipment ready to be deployed into an outbreak situation. It needs to be there as soon as these sorts of outbreaks occur. It needs to be on the ground. We need to have people ready and trained to be able to get the data analysed and made available to the public health authorities.
- Previous The history of blood letting
- Next How sitting harms your health










Comments
Add a comment