Immune Attack of Cancer Cells
Interview with
Chris - And now, to cancer and how to persuade the immune system to attack it, Alexandre Corthay.
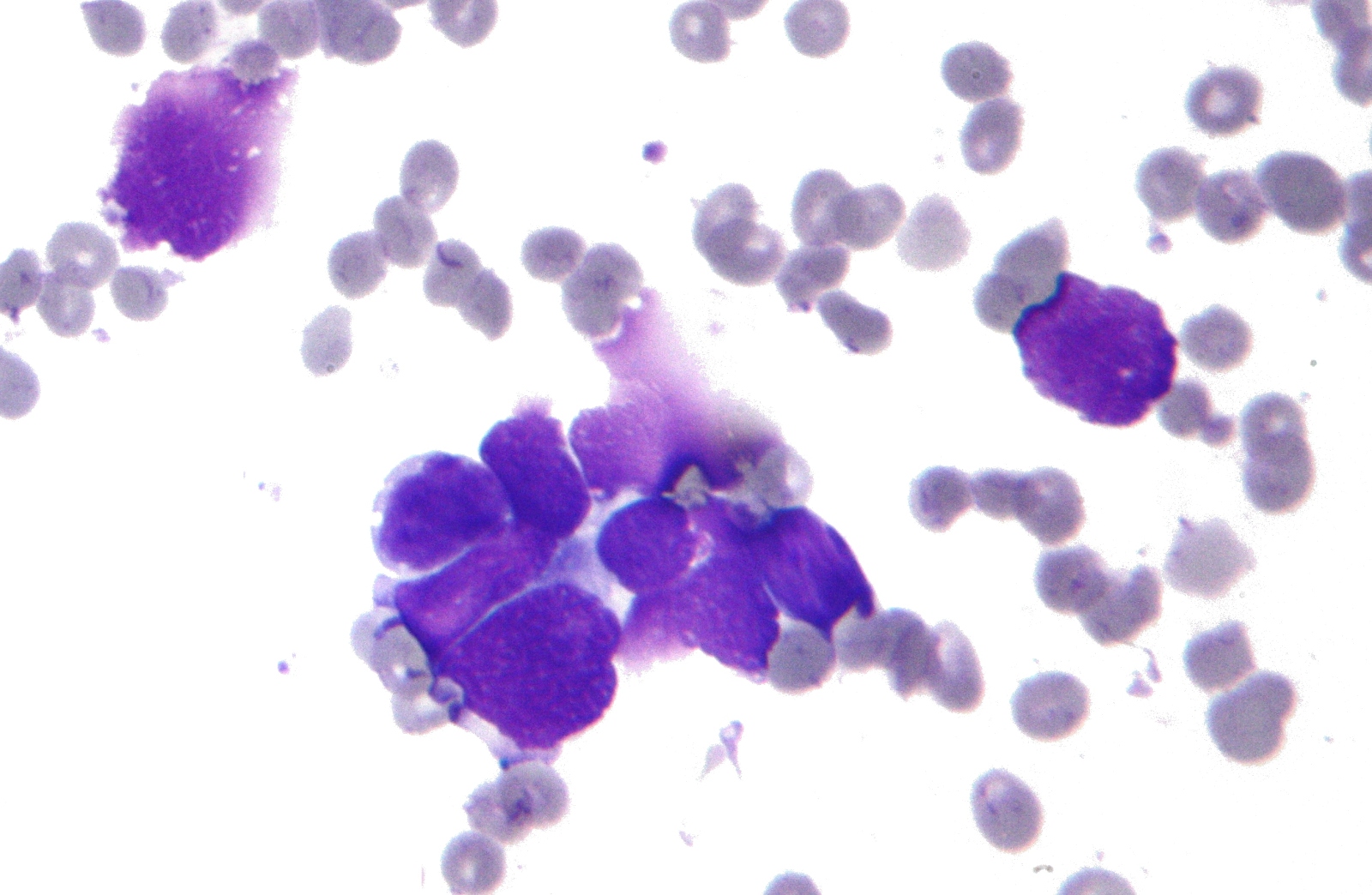
Alexandre - We know that the immune system protects us against cancer, but there is still very little known about how this immune system protects against cancer and this is what we are trying to find out. We are using an experimental system in the mouse. The type of cancer we are studying is a bone marrow cancer, it's called multiple myeloma and also lymphoma. We're interested in immune cells called T-helper cells, so we're interested in how T-helper cells fight cancer.
Chris - Can you talk me through the experiments you've been doing in these mice to work out how the immune system usually protects them and what goes wrong when the cancer occurs?
Alexandre - What we think is going on when people develop cancer is not that there is anything wrong with the immune system. What we think is going on is that the cancer cells somehow manage to fool the immune system to evade the immune response presumably by producing molecules that will suppress the immune system.
Chris - When a cell becomes cancerous, how does the immune system pick that up normally and remove that cell to stop a cancer occurring?
Alexandre - There are two major ways. One way is by recognising stressed cells. So any stressed cell in your body will show it on the cell surface. There are some stress markers and that will be recognised by the immune system and the immune system will simply kill the stressed cells. The other way, which is even more refined, is that the immune system is able to recognise mutations in self. Mutations that are required for normal cells to become a cancer cell. There is a certain number of mutations in the DNA that are required and the immune system is able to recognise, not directly the mutations, but the effect on proteins.
Chris - And any cells displaying that sort of danger signal are just going to get deleted straight away.
Alexandre - Exactly.
 Chris - But obviously, not all the time because otherwise no-one would get cancer.
Chris - But obviously, not all the time because otherwise no-one would get cancer.
Alexandre - So, most of time - so that's why most of us do not have any cancer. It's also probably the reason why it takes so many years to develop cancer. Usually, people develop cancer after the age of 50, so we are extremely well-protected against cancer. But sometimes the cancer cells manage to evade immune response.
Chris - And how do they do that?
Alexandre - It is not well-known yet, but one major way to do that is to use the communication system that the immune system use. So, immune cells communicate with each other and cancer cells are known to produce some signal molecules that the immune system use normally to suppress itself. At the end of a normal immune response, the immune system shuts it off and this is probably what the cancer cells do - they tell the immune system to shut off.
Chris - So by chance, the cancer evolves the ability to produce some of the chemicals that would normally damp down the immune response, thereby, effectively putting it under the immune radar. It's just looking like healthy normal tissue to the immune system or it's basically suppressing the immune system where the cancer is, stopping it being destroyed.
Alexandre - That's absolutely correct, but I should stress that there are some very good indications that the immune system never gives up. So even in a cancer patient with established cancer, the immune system still fights back and there's a battle going on in the cancer patient. This is very important because it means that it should be possible to stimulate, to help the immune system to tip the balance towards cure of the cancer patient, and this is something we really hope for the future.
Chris - Well, people have been working on the field of immunotherapy where the idea is you would take some of the tumour out of the patient, take immune cells from the patient in the dish and use growth factors to try and drive the immune cells very hard to overcome whatever that inhibition is coming out of the tumour, and sometimes you get immune cells that will attack the tumour, but often not. Because there have been a few case reports written up of people who have had complete remission of cancers that way, but all too often, it doesn't work.
Alexandre - Yeah, so this is called - what you're mentioning is called adaptive T-cell transfer. So culturing T-lymphocytes in vitro and then giving them back to the patient and this has shown some very promising effects. One key issue there which is also valid for the development of cancer vaccines, is to know what type of immune response to trigger. Many different types of immune responses are used by the body against various types of infections or cancer, and it is still not very clearly known what is the right type of immune response that is the best to fight cancer, and this is what we're working on.
Chris - What have you found so far?
Alexandre - We have found that, in a certain mouse model, that the optimal immune response to fight cancer is an inflammatory immune response driven by the type of T-cells called TH1 cells.
Chris - And if you could induce that in people who have a cancer where the immune system is not combating it, would that push the cancer into remission then?
Alexandre - This is our prediction. This would be the two arms of the immune system to stimulate - in one way, to stimulate an inflammatory environment especially in the tumour which will be very important to recruit immune cells, particularly T-cells and the other important aspect is to stimulate TH1 cells which recognise very specifically the cancer cells and which tell other cells to kill the cancer cells.
Chris - What about risks though because one worries that if you get the immune system attacking, what is self-tissue? It's your own body. There's a concern that the immune response might spill over and become mistargeted away from the tumour and at healthy tissue and you then end up with an autoimmune disease.
Alexandre - That's correct so that one should be always very careful when triggering the immune system because as you said, the immune system is very potent. It may trigger autoimmune diseases, it will also kill you if the immune response is too strong. However, cancer is definitely very dangerous to people. Cancer is killing people and on the other hand, current cancer therapies are also very tough to the patients like chemotherapies, and irradiation. So, I think there's always a balance, but I can really see a future where immunotherapy will be perfectly developed and will help the patients with minimal side effects. But of course, when you treat a serious disease, it is very difficult not to have any damaging effect on the patient at all.
Chris - And the results you've got in the mice with the haematological tumours, will that transfer directly to other kinds of malignancy?
Alexandre - We cannot say that yet, but in my view yes, and from the literature, not much has been done at that level of details. But it looks very much like this is a general way of how the immune system fights cancer. So this TH1-driven inflammatory response. That's my expectation that this will translate to other types of cancer and also to humans.
Chris - Alexandre Corthay.










Comments
Add a comment