COVID Vaccines Explained
As the UK surpasses its goal of vaccinating 15 million people by the 15th of February, we're taking an in-depth look at COVID vaccines: how they work, what efficacy really means, and will they protect us against viral variants? Plus, in the news, updates to the list of COVID symptoms to watch out for; Chris Packham on the animal Einsteins giving humans a run for their money; and how scientists are using whale songs to explore the ocean floor...
In this episode

00:57 - COVID symptoms: REACT study identifies new giveaways of infection
COVID symptoms: REACT study identifies new giveaways of infection
Joshua Elliott, Imperial College School of Public Health
Last year, a “holy trinity” of symptoms - cough, fever and sudden loss of smell and taste - were introduced as the cardinal giveaways that someone might have coronavirus infection and they should go and get a test. Since then, other symptoms have been documented, but they’ve not been regarded as adequately specific to warrant inclusion: too many people, it was felt, might suffer false alarms. But, at the same time, we’re currently missing a significant number of cases, and with the emergence of new variants of the virus, might the symptom list be in need of an update? Josh Elliott thinks so. He works at Imperial College’s School of Public Health...
Josh - One of the main reasons for doing this study was to find what were the most informative symptoms for whether or not you have COVID. Currently you are eligible for community testing if you have one of three symptoms: loss or change to your sense of smell or taste, a fever, or a new continuous cough. And our study, we considered loss of sense of smell and loss of sense of taste as different symptoms. We find that all of these symptoms are the most important symptoms for predicting your risk of COVID. However, there are additional symptoms that we identify which give extra information on whether you have COVID or not - your risk of COVID.
Chris - We can come to those in just a second, but can you tell us, first of all, how you actually did this?
Josh - We use data from a study called REACT 1 which stands for Real-time Assessment of Community Transmission, One. Roughly every month 160,000 people are included, which is a random sample of the English population five years plus. In every single individual, we have a PCR test result, we have information that they give us from questionnaires including about their age, their sex, their ethnicity, et cetera, as well as any symptoms. From that data we can make models which show which symptoms provide important information as to your risk of COVID.
Chris - What's interesting is that you've studied this across the time when we've seen the emergence of new variants of coronavirus in the country. So did you see any difference in what we'll call the classical coronavirus, the parent, and then the new virus we're now seeing?
Josh - So we indirectly studied the new variant by looking at a round that took place in January 2021, when over 80% of positive tests were due to the new variant versus a round which occurred at a similar seasonal time in November and December when the proportion of positives were only around 15 or 16% due to that new variant. And in doing this, we could find that loss of sense of smell was less predictive for the later round in January than in the earlier rounds. And also we found that the new persistent cough was more predictive in the January round than in the November/December round.
Chris - So basically with the new variant you cough more but you can taste your dinner better than you would have done had you had the existing parent virus. Why do you think that is?
Josh - It's difficult to speculate exactly. It might be something to do with the way that the virus interacts with the lining, where chemicals have attached to the lining of your nose so that you can smell, or it might be to do with the way that the virus levels are just higher in infection. It's not clear at the moment.
Chris - And what about the other symptoms that you were looking up? Cause obviously you're giving questionnaires to people, you're extracting a lot of data. So in addition to that magic number of four symptoms that you looked at, were there any other really good predictive symptoms that would steer us towards a diagnosis of coronavirus in people who had them?
Josh - Yes, and one key thing I want to stress about these symptoms that I'm about to list are that they provide additional information alongside those other four symptoms. So it's only when you consider all of these together that you're getting the most out of them. So those symptoms were across all ages: chills, headache in children - so people aged 5 to 17 - appetite loss in adults of any age, and muscle aches in adults aged between 18 and 54. So all of those are adding extra information to tell us about your risk of COVID based on what symptoms you have
Chris - With the list of symptoms that you've found are any emerging as ones that perhaps we should consider adding to the three or four cardinal features that we're using to trigger people to go and get a test? Because the government have been quite resistant about this. They were asked about this last year, should we extend the definition of what constitutes someone who might have coronavirus? And they felt that they shouldn't do that because it would end up leading to too many people suspecting themselves of coronavirus when in fact they didn't have it. From your data. Is there evidence that perhaps we should have more symptoms on that list?
Josh - Yeah. So of all the people that has any one of the four symptoms overall, you're only picking up about half of the overall number of symptomatic infections in the community. You would get from halfway to three quarters of all symptomatic cases in the community if you used our suggested models. In order to do that, you would have to offer tests to 2 and a half times the numbers of people in the community.
Chris - So in other words, the price to be paid for having a wider definition is we have to do more tests because we're going to drag in more people who haven't really got coronavirus. We have to test them to prove they haven't. But at the same time, the payback is we could, potentially, instead of missing half of cases, we'd miss far fewer positive cases because we would end up testing more people and finding them.
Josh - That's true.
Chris - What have the government said when you present them with this, are they likely to embrace this and to include your symptoms that you're identifying as a way to find more people? Because this has proved to be a real headache, hasn't it, tracking down, pinning down the virus because at the moment we miss too many cases and it makes it very hard to control.
Josh - Yes, I do think that we need to do something in order to reach more people that might have the virus and also coming forward and wanting testing, but currently aren't eligible. And I do think that there is interest from the government in updating the eligibility rules for testing in the community.

07:01 - Depression susceptibility passed down through sperm
Depression susceptibility passed down through sperm
Rahia Mashoodh, University of Cambridge
We look like our parents because we inherit DNA from each of them, and that DNA is the recipe book that controls how our bodies put themselves together when we’re embryos. But, it turns out that other traits can be transmitted from parents to their offspring too, but not directly in the DNA. Researchers in China have shown that male mice that become depressed can pass on an increased tendency for depression to their offspring. The scientists speculate that pieces of short-lived additional genetic material, made of a chemical relative of DNA called RNA, are added to the sperm in the depressed dads. When these sperm fertilise eggs, the RNA messages alter which genes are turned on and off early in the animal’s development, switching its susceptibility to depression. Rahia Mashoodh wasn’t part of the study but is involved in similar research at the University of Cambridge...
Rahia - So what they did was they took mice and exposed them to a chronic stressor. And what this did at the end of the 5 week period, these mice started to show what scientists would call sort of depression-like behaviour. Obviously mice don't get depressed in the ways humans do, but there are things we can test in mice that tell us that they are showing very similar symptoms. And so they do this and then they ask actually, can this experience be transmitted to the next generation? And they take females that don't have such an experience and they get mated with these males. And then they look at their offspring and their offspring seemed to be fine. If you have a depressed father, you have an offspring that seems to look like a normal, healthy, happy mouse. However, they seem to be predisposed to stressful stimuli. So for example, when you then expose them to a stressor, they start to show behaviour similar to their father so depression-like stressed behaviour.
Eva - I see, so essentially, if you stress out one of these mice, they're more likely to start having depression-like symptoms after maybe fewer stresses than a normal mouse might have?
Rahia - Exactly. What that suggests is that what these fathers have conferred is like an underlying variability to that stress-related behaviour.
Eva - How did they then go about figuring out how that was transmitted?
Rahia - So what they were interested in was the idea that maybe there's something in sperm that gets transmitted during development, because mouse fathers don't really participate in the care of their offspring. So what else could fathers be transmitting? They thought that it must be in the sperm. And so they look at what's called small non-coding RNA. And these are molecules that come from your genes, but basically have regulatory functions. So they bind to other genes and inhibit their expression, and so they can cause a wave of change. So what they decided to do is first look at what's in the sperm, and they found a bunch of changes in these small RNAs. And then they wanted to say: is what's in the sperm actually sufficient to cause the effects they see in offspring? And so they essentially did what's called artificial insemination, where they took the sperm, implanted it into an egg, and then implanted it into a mother. So the mother has no idea who she's mated with, and it just gets transmitted directly. And they found that again, in vitro fertilisation was sufficient to create offspring that were hypersensitive to stress. The crucial bit is that these experiments were performed in genetically identical individuals, and so the only thing that could vary is the expression of these RNAs.
Eva - How does stressing out a male mouse lead to different kinds of RNA in the sperm that he makes?
Rahia - One of the theories about this is that the sperm production happens in the gonad, and because stress can be so systemic, the stress hormones reach the gonads. And they then cause various effects along the sort of sperm track. And as they're traveling, they pick up all of these small RNAs... we still don't know.
Eva - Once the sperm with the depressive RNA reaches the egg, what does the RNA actually do in the egg to cause the effects in the embryo?
Rahia - These small RNAs - their entire function has to do with regulating gene expression. And so what these authors basically show is that when you inject these small RNAs, you're basically changing all of the gene expression - or the gene expression profile - of the developing embryo, and it's setting the trajectory of how that embryo will develop. And a lot of the genes that are being affected have to do with brain development and stress-related circuitry.
Eva - How many generations, then, did they track whether or not this effect was carried on? So - was it just in the babies, or the grandbabies, or the grand-grandbabies as well?
Rahia - What they find is that this only persists to their offspring. And so it's very short-lived.
Eva - How far can we say this might be true for humans too?
Rahia - There have been some studies looking at human sperm, particularly in the context of poor diet, showing that there are differences in the sperm that mirror some of these effects that we've just talked about. And so I think the capacity for them exists, but I think it's also important to remember that humans aren't lab mice, and so they live in very complex environments where there are many competing factors for these things. And so we don't really know when something like this would be transmitted or not. We're also slightly genetically different from one another, and so in these mice, because they're so identical, it is possible that these effects might be more prominent. And what we don't really know is how different underlying genotypes interact with these types of effects.

14:16 - Chris Packham's Animal Einsteins
Chris Packham's Animal Einsteins
Chris Packham, Naturalist and Broadcaster
A new nature show is coming to the BBC - called 'Chris Packham’s Animal Einsteins!' And Chris Packham came to tell us more...
Chris - We thought we'd take some snapshots at the latest science regarding animal cognition. We've been a bit generous with cognition, so we're looking at animals which, anthropomorphically at least, appear smart and clever to us. Some of their adaptations, both behaviourally and physiologically, are quite astonishing. But we've also focused on the new science that's coming to the fore about cognition, and also those species that we're familiar with. So we've looked in particular at some domestic animals, which we like to think are smart, but for a long time science has been telling us they're not as smart as we like to think they are! But it turns out that we, as opposed to the scientists, could have been right all along.
Eva - What was your favourite, smartest animal that you had a look at then?
Chris - I'm a dog lover; I've got a couple of poodles. I keep poodles because allegedly they're amongst the two smartest breeds of dog. But as you probably know, they have never passed what we call the mirror test. Now the mirror test is where an animal can look into a mirror and recognise its reflection as itself. So when Nancy, my poodle, looks into the mirror, we don't honestly know whether she recognises another dog, another poodle, or Nancy. But a scientist in America has just done a neat bit of work; he took his dog out for a walk in the snow around a regular route, and the dog - as you know - will urinate, they'll mark their range; and then he took the dog home. He went back out with a bucket and a spade and he moved some of the yellow snow, the dogs urine - which we know is particular to each animal, it has an individual scent - and then he moved it around the route, and then took his dog for a second walk. And what he found was that when his dog encountered its own urine, but in a place where it hasn't deposited it, it became extremely agitated. And what we are now postulating is that dogs might manifest a sense of self, a theory of mind, but not in a visual way. And that might make sense. Dogs are not terribly brilliant when it comes to their eyesight - they're dichromatic, they see with the equivalent of human male red-green colour blindness, but their sense of smell as you know is profound. So it could well be that we have been rather blinkered, if you'll forgive the pun, when it comes to looking at these creatures and assessing their intelligence, and it could be that they are manifesting that and using it with a different sensory capability than we can relate to.
Eva - Amazing - so they're not visualising themselves being somewhere, they're smell-o-rising themselves as being in a different location!
Chris - Exactly. They know themselves through smell, not through vision. We've tested this previously with dolphins. Dolphins in captivity have had a little bit of lipstick put on top of their head. They swim up to the mirror, they twist and they turn, they see the lipstick and then they swim off and try and wipe it off. So quite clearly they know it's them. But what's also interesting is that experiment, with the little mark on the head of the animal and a mirror, has just been performed with a tiny fish, a reef fish called a bluestreak cleaner wrasse, and it passed the mirror test. So this tiny little fish understands, when it looks into the mirror, that that is it as an individual. And of course the repercussions of this are quite profound, because if you know yourself as an individual, you will know all of the other cleaner wrasse, perhaps other species of fish, as individuals. And that means understanding their characteristics and personalities. And the more you can analyse that, the better it is for you; the greater advantage you can take of their strengths and weaknesses.

18:01 - Using fin whale songs to find out what's below the sea floor
Using fin whale songs to find out what's below the sea floor
Vaclav Kuna, Institute of Geophysics of the Czech Academy of Sciences
Adam Murphy’s been looking into how whales singing as they travel through the water may hold the key to a more environmentally-sensitive way to search for oil and gas and see what’s happening under the ground, as he heard from researcher Vaclav Kuna...
Adam - Finding out what is under the ocean floor is serious business. It can tell us more about our planet, sure, but it also helps us find deposits of gas and oil. One of the best ways to do that is using sound, like sonar. Sound travels at different speeds through different materials. And at the boundary between two materials it can change direction, or even reflect off of it. So the sound from one source can reach its destination through a load of different ways. And by mapping out all those different ways as they come in, you can start to get a picture of what's going on under the surface. But it's not easy, and the way to generate that sound is somewhat dramatic. Right now we use air guns - big underwater explosions - to give us the noise we need. And it disturbs sea life and has been linked to a whole host of negative effects. But what if there was a way to work with that sea life instead of against it? Well, Vaclav Kuna from the Institute of Geophysics in Prague may have spotted a solution.
Vaclav - When I saw those whale calls and I saw the characteristics of the whale calls, I noticed that there are some signals that I couldn't really explain - those echoes. And it came to my mind that those may be actually those subsurface signals, and then t was quite easy for me then to say, "Hey, maybe we can test out this seismic imaging method on this"
Adam - Fin whales are relatives of blue whales and they sing as they travel, like this song which has been sped up by 10 times.
[whale song]
And they're loud, loud enough that you might be able to map under the ocean floor as they're travelling along.
Vaclav - So the highest energy wave, the call comes straight from the whale to the station. Then there are other kinds of waves or reflections of the direct wave. It's a wave that goes from the whale down to the ocean bottom, and then it bounces off, travels to the ocean surface and bounces again and travels to the station. And then there are other waves - phases as we call them - that goes down to the ocean bottom. And when it meets the ocean floor, it actually penetrates through the floor. It goes in the sediment layer and then it either bounces off or sometimes it even penetrates that and goes even deeper. And those waves, eventually they either bounce off or kind of like turn slowly back up and we can record them on the ocean bottom seismic station.
Adam - And although the whale calls don't have the same resolution as the airgun approach, doing it this way has its advantages.
Vaclav - There is a few reasons. First of all, they are for free and they are pretty much globally spread. So it's kind of a win-win that we have some signals already recorded somewhere and we don't need to pay for them. And also there's a very long on-going debate about the traditional seismic surveys that may be harming ocean mammals because they produce very loud sounds. So yeah, we don't really want to add more noise in the ocean if we don't have to.

23:17 - How does a vaccine work to protect us?
How does a vaccine work to protect us?
This week COVID-19 vaccines are going under our microscope; we’ll hear how the different vaccines work, how they have been tested and what 90% or 70% efficacy actually means, how scientists know whether they work against viral variants or not, and whether vaccination passports are on the cards in future...But first, how do vaccines actually work? Katie Haylor explains...
Katie - Vaccines work by showing the immune system what a foreign invader looks like before we meet it for real. This enables us to build an immune response, made up of white blood cells, called T cells, that can recognise and kill-off cells harbouring viruses, and sticky molecules called antibodies that can glue themselves to critical parts of infectious organisms, preventing them from causing further trouble. To make this happen, the body needs to be exposed to either the whole virus or bacterium, or to some of the critical pieces that make that infection tick.
It takes about 2-3 weeks after vaccination for the response to begin to develop. The immune system also stores the instructions for how to make this response in a population of “memory cells”. These are very long lived, so if we encounter the same threat again at some later time we can often use this memory to rapidly mobilise the same effective response. Crucially though, this time, it happens much faster, so we get on top of the infection before it gets on top of us. This is the “immunity” that we get from a vaccine. But like anything that activates the immune system, vaccines can sometimes produce side effects similar to the infection itself. Chills, headaches and muscle aches sometimes happen, but these are almost always mild and short-lived.
24:46 - Vaccine efficacy: how well does a vaccine work?
Vaccine efficacy: how well does a vaccine work?
Stephen Evans, London School of Health and Hygiene
In the present game numbers are everything, and here to unpick them for us is Stephen Evans, a medical statistician at the London School of Hygiene and Tropical Medicine, speaking with Chris Smith...
Stephen - In my area of about 5,000 people, over the next week there could easily be a hundred people who end up with Covid-19. If they're unvaccinated, then those hundred people will get the disease. If they're vaccinated with a vaccine with a 90% efficacy, then 90 of them will be protected from getting any symptoms of the disease. There will be 10 who will still get symptoms. Some of those 10 may be protected from more severe disease, but that's what the 90% means. It doesn't mean that each individual is 90% protected, but about 90% of the people who would otherwise get it are protected and 10 are less protected.
Chris - The values we're looking at for AstraZeneca's vaccine are somewhere hovering around 80%, aren't they? And the values returned for Pfizer's vaccine, after two doses, are said to be in the region of 95%. So given what you've just told us, if I have a vaccine that's for the sake of argument, let's say 95% effective, and that means that five and every hundred people won't be protected and could catch it. Does that mean then that a person getting the AstraZeneca vaccine is in theory worse off than someone getting the Pfizer vaccine because they've got a higher likelihood that they might not be protected?
Stephen - Yes, there is a slightly higher risk of getting mild disease. Whether there is any extra risk of being hospitalised and getting severe disease, we don't fully know, but it's quite likely that the AstraZeneca vaccine will still protect - even those who get mild disease are unlikely to be hospitalised or die.
Chris - What do you think is going on with the Europeans then? Because our MHRA gave the AstraZeneca vaccine the nod. The equivalent across Europe, the EMA, also approved its use. But then some countries said that they wouldn't be approving it for older people because they didn't have enough data, they're saying. And this has obviously led to a number of people being quite concerned who are in the older age bracket and were destined to receive or have received AstraZeneca's vaccine. What should they take away from this information?
Stephen - You need to distinguish approved and prioritised. If you have plenty of the AstraZeneca vaccine and plenty of the Pfizer vaccine, then you might need to decide, "who will we prioritise?" And so it is reasonable to say, we will prioritize the Pfizer vaccine to the elderly if we have plenty of it, because we have better evidence in the elderly. Now it doesn't mean that the AstraZeneca doesn't protect them. It's just that the trials didn't have enough people who caught the disease to be able to demonstrate that you didn't get mild disease. But the data on the antibodies that we just heard about, and the data on the T cells and B cells, suggest that the elderly will be protected just as much. So that's why the EMA and the MHRA have said these are authorised in older people. So there is no need to be concerned that they don't have efficacy, but you need to prioritise depending on the context you're in. And we have lots of people in care homes who would not find it easy to get the Pfizer vaccine because of its cold chain. And so our decision to give them the AstraZeneca vaccine is eminently sensible.
Chris - And South Africa have stirred up some controversy because they're sitting on million scale numbers of doses of AstraZeneca's vaccine and have called a halt to its rollout citing, as far as we know, one small trial from the University of Witwatersrand where the average age in that trial was 31. And there were no people in it who got severe disease, but they said they didn't feel that it was adequate data in terms of the protection confirmed by AstraZeneca's vaccine to use it. Where do you think they're coming from?
Stephen - I think that's very strange. I think that if you're then going to say that I'm happy to have a whole lot of people who die unprotected by any vaccine, that's a very strange decision to make. Okay. It's entirely possible the AstraZeneca vaccine will be less effective, but making comparisons between vaccines is very difficult when you haven't done the actual comparison.
30:06 - Viral vector vaccines: what are they, and how do they work?
Viral vector vaccines: what are they, and how do they work?
We heard earlier how vaccines work in general, but there are differences between how they achieve their protective effects. AstraZeneca’s vaccine is what’s called a viral vector vaccine, and here’s Adam Murphy to explain how it works…
Adam - Vaccines rely on showing the immune system what a potential infection “looks” like. One way to do this is to “smuggle” the genetic message for making a few key parts of the infection into the body, and then to rely on our own cells decoding that message and making the pieces of the infecting organism themselves. When they do this, the pieces are presented to the immune system as though the infection were there, growing in the body for real, and this can produce a very powerful response. Of course, the infection isn’t really present so this is a very safe approach. The question is how to get that genetic message into the body in the first place. And it turns out that, because viruses themselves have naturally evolved to be very efficient at invading and hijacking our cells, they make excellent Trojan Horses - or vectors - for doing just this.
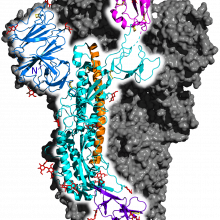
So scientists take a virus, and first disable it by removing its own genetic instructions that tell it how to grow. This means it’s harmless in the body. They then add the instructions for making - in the case of the coronavirus vaccine - the “spike protein” that the coronavirus uses to get into our cells when it infects us. This means that, when the disabled virus is injected into the body, it penetrates our cells, and although it can’t itself grow, it does cause the cells to temporarily churn out pieces of the outer coat of the coronavirus. These are presented to the immune system, and trigger it to produce a protective response.
AstraZeneca’s vaccine works this way, as does the Russian Sputnik V vaccine, and Janssen’s vaccine, which all use disabled cold viruses to carry the coronavirus spike message into the body. These vaccines tend to be very safe and very easy to store and transport. But one downside is that, because they use a virus to carry in the coronavirus message, the immune system will also react to the viral vector itself, potentially limiting the number of times they can be used in the same individual…

32:30 - COVID variants and vaccines
COVID variants and vaccines
Zania Stamataki, University of Birmingham
In general, vaccines protect us against specific threats. But if that threat changes or mutates, the vaccine needs updating. This is why we periodically need to alter what goes into the flu vaccines we use each year. And the new coronavirus is no exception. In recent months, “new variants” of the virus have been picked up in several countries, and concerns have been raised whether these variants might be able to side-step the protection we’ve received from vaccination. Zania Stamataki is a viral immunologist at the University of Birmingham, and spoke with Eva Higginbotham...
Zania - Viruses replicate rapidly and if they stayed the same, then our immune system would vanquish them very, very quickly. And that's why they have evolved the ability to mutate. And the coronavirus that causes COVID 19 mutates once or twice a month. When these mutations lead to a virus that has different properties than its predecessor, then it's called a variant.
Eva - We think the coronavirus mutates once or twice a month, is that quite a fast replication in terms of viruses, or is that quite slow?
Zania - Compared to influenza, the flu virus, it is slower. It's a slower mutating virus. But generally mutations of once or twice a month can be considered significant enough for us to keep surveillance on an annual basis. We don't know when the new mutation is going to lead to a new variant, which means that the virus will have different properties. So we need to keep an eye on these things.
Eva - Why might these mutations and these new variants have an effect on the vaccines that we've made?
Zania - So vaccines that use viruses as blueprints to educate our immune system so that when we are infected, we have pre-existing defenses. When vaccinated, we make strong antibodies and T-cell responses against proteins of the virus that are harmless. If the variants are too different from the viruses used to make the vaccine, then we will need to update the vaccine with the new blueprints to the new virus.
Eva - And how can we tell if a vaccine is still going to work against a new variant? What kind of tests can we do to ensure that we're using vaccines that are actually going to work on the variant that's circulating through a population?
Zania - Well, public health officials monitor the incidence of disease, hospitalisations, and deaths in vaccinated people. And this is how we monitor effectiveness against new variants. But in the lab, we can test this very, very quickly. We can take a sample of blood, and we test to see if your antibodies and your T-lymphocytes, your T-cells, are effective against the variant. Antibodies raised by current vaccines were less effective against the South African variant, for example, which means that we had to use more of these antibodies to neutralise the virus in the lab. They weren't completely ineffective though.
Eva - I see. So it doesn't mean that the antibodies just don't recognise the virus at all. It just means that they recognise it slightly less. And so we need more antibodies in order to get a good effect.
Zania - Exactly. And it's very important also to remember, that just as the virus evolves, so does our immune system. So in natural infection, when a new virus variant emerges, our body will respond by making new types of antibodies to cover this new variant. And this is what we're going to try and do with vaccination as well, going forward, we're going to keep an eye on it, and we're going to update the vaccines to make sure that they are effective in the future.
Eva - Can we try and get ahead of the problem like we do with the flu vaccine, where basically every year, some scientists try and work out what variant of the flu is going to be the most problematic in the year to come. And so then we designed the vaccine against a predicted model of what the virus might look like. Can we do that for coronavirus and try to get ahead of the problem?
Zania - Absolutely we can. And we are doing this already. And just like with flu, there are virus hunters. They are sequencing viruses around the world every season, to update our vaccines for influenza. We need to keep surveillance on this coronavirus too. And the new vaccine technologies that we currently have, allow us to respond rapidly with new vaccine recipes. As individuals, there is something that we can do as well to make sure that our vaccines work for longer. We can continue to take steps to reduce transmission, and keep any new variants emerging in our own bodies to ourselves. We all know how to do that.
36:56 - mRNA vaccines: what are they, and how do they work?
mRNA vaccines: what are they, and how do they work?
The first vaccine to make it across the line internationally and go into patients outside of a trial was the Pfizer vaccine. It’s what’s called an mRNA vaccine; we’ve never made a vaccine like this before. So how does it work? Martin Khechara explains...
Martin - Another way to show the immune system what an infection might look like is to introduce pieces of the genetic material from the infection directly. This is how the Pfizer and Moderna vaccines work. It’s brand new technology that has never been used to make a vaccine in humans before. Scientists there have taken a short piece of the coronavirus RNA genetic code containing the instructions for the spike protein that the virus uses to latch onto and invade our cells. Rather than put this into a disabled virus to get it into the body, they’ve instead wrapped up the pieces of code in tiny droplets of oil. When they’re injected, these stick to the surfaces of nearby cells and, just like two soap bubbles that stick and merge together, the oily droplets fuse with the cell surface and discharge their genetic cargo inside. The cells then read the genetic code and use it to produce large amounts of the coronavirus spike protein, provoking a protective immune response. The genetic material is eventually degraded in the cells, bringing the process to an end. Because these vaccines tend to be less robust than viral vectors, and they can be harder to make, they tend to be more costly and can also be more difficult to store and transport, which can limit their use.

38:31 - COVID vaccine trials in children and immunocompromised people
COVID vaccine trials in children and immunocompromised people
Rajeka Lazarus, University Hospital Bristol and Weston
In recent weeks the UK government has announced a £7M initiative to look at the potential value of mixing and matching different vaccines. Trials are also underway to look at how well the vaccines perform in children, who were not included initially, and also among people with compromised immune systems. Rajeka Lazarus, from University Hospital Bristol and Weston, is running several of these, and spoke to Chris Smith...
Rajeka - So the main rationale is to improve the flexibility and ease by which the vaccines can be delivered, so that as many people as possible can be vaccinated. So what this means is if you've been vaccinated with one type of vaccine, and you're ready to have your next dose, if your local centre actually doesn't have that, then it's going to be more difficult, or more time consuming for you to get the same dose as you had before. So that's really the main reason. The second reason is that there may be some advantages in having the different types of vaccines. They may compliment each other, and actually enrich the immune response overall.
Chris - Do we have evidence that that's actually the case, because arguably some people who are being recruited into this trial could say, well, actually, that doesn't sound good if you don't know for sure. So I won't take part.
Rajeka - So we do have some evidence so far, that has been found in animal studies, where they have given the different types of vaccines together. And actually it did show by having two different vaccines, you get a richer immune response, and a higher antibody concentration compared to having two of the same vaccine type. So that is promising. And what we're looking for in this study really, is not that the two different vaccines make a better response, it's that they don't make any response that's less than two of the same doses.
Chris - There's also some question about whether or not some of the vaccines that are being used, can be used more than once, because the vaccines are themselves a virus, and this will elicit an immune response on the part of the recipient. And some are arguing this could therefore be a safeguard on the part of our ability to defend the population, because we may have to use different vaccines in people the next time they're vaccinated going forward. So knowing this information up front is very helpful.
Rajeka - Yeah, that's absolutely right. There have been a small number of people who received these viral vector vaccines that you've heard talked about. For other infections, for studies done in Oxford who have been part of the trial, and have found to be, have adequate responses. But we do need more information.
Chris - You're also looking at children now, some may say, why didn't we look at children in the first place? And also if children are at such low risk, which has been the policy headline along the way, children don't seem to get this very severely. They don't seem to pass on the virus very often. Why are we now vaccinating or worried about vaccinating children?
Rajeka - I think it's quite usual practice to test out new vaccines and other products in healthy adults first, and then move on to other groups who may benefit from vaccination. Although children are lower risk, they're not at no risk. And there may be some children who are more vulnerable than others. And we do know that children can get COVID, and they can get post infection syndromes that can make them quite poorly. And it's also thought that, certainly with the new variants, they are transmitted as effectively in all the age groups. So it may be that children are involved in transmitting the virus within the community. So if we do want to stop transmission, we need to look at vaccinating children.
Chris - The other group who are also concerned, are people who have a poorly functioning immune system, the so-called immunocompromised. People who are on drugs that suppress their immune system. People who've had organ transplants, bone marrow transplants. They may have some inherited problem with their immune system, or disease like HIV. So their immune system might be broken for that reason. They haven't been formally studied so far, have they, as a group to see how they respond to the vaccine? So how are you trying to learn what sort of advice we can offer to somebody who's in that situation? They're a bit immunocompromised or a lot immunocompromised, and they'd like to know what their prospects are having had the vaccine.
Rajeka - So that's right Chris. The studies haven't been done in this group of people with problems with their immune system. And I think that the main thing to say is that these vaccines are safe. They're not live vaccines. So they shouldn't cause you any problems if your immune system is compromised, but we still need to establish how well they do work. And there are studies that have been started in the UK to follow-up people with different types of immune system problems, to establish how well they're working, to then work out whether people may need a different type of vaccine, or more doses, and work out how best to protect people with these problems.
Chris - And to finish us up here, Rajeka, what do we know yet about how long the immune response lasts for, in response to these vaccines? Because obviously we don't have time machines. We don't have crystal balls, we can't see into the future. So we really only know a bit about the time since we've been giving the vaccine. So what do we anticipate will be the length of protection, because that will obviously inform what we decide to do next in terms of boosting people and so on.
Rajeka - Yeah. I think that is a difficult question to answer at the moment, but the information is being collected. So the first people to start, certainly in the Oxford vaccine study, started a study last April, May. So we are coming on to close to eight, nine, ten months. So we will have some information. I think it's reassuring that we can see from the Oxford study, that a single dose provides good protection that persists for the 12 weeks. And we know that the booster dose will then produce a higher antibody response, which should then last longer.
44:28 - Protein subunit vaccines: what are they, and how do they work?
Protein subunit vaccines: what are they, and how do they work?
The drug company Novavax recently announced the results of their new vaccine, which is known as a protein subunit vaccine and, incredibly, uses technology based on insect cells, as Eva Higginbotham explains...
Eva - One of the most tried and tested forms of vaccination is called a protein subunit vaccine. This is where large amounts of one part of a virus are produced in culture in the laboratory, purified and then injected into the body. The hepatitis B and the cervical cancer vaccines are made this way. And recently the company Novavax announced they’ve developed a method to do this for the new coronavirus. They add the gene for the coronavirus spike protein to insect cells grown in the laboratory dish. The cells churn out large amounts of coronavirus spike proteins, which clump together and can be easily separated and purified into a vaccine. When they’re injected, cells nearby pick up these proteins and present them to the immune system, producing protective antibodies within a few weeks. This is a very safe technique that is also easy to scale up and the resulting vaccine is easy to transport and store. But one downside is that it does tend to produce mostly antibodies rather than white blood cells, which might make the protective more short-lived and potentially less effective against variants of the virus.

45:54 - COVID vaccines: questions for the future
COVID vaccines: questions for the future
Vijay Samant, Brickell Biotech
And finally, what is the future of covid vaccines? Vijay Samant has years of experience in overseeing companies as they develop vaccines and is currently the director of pharmaceutical company Brickell Biotech. Chris Smith spoke with Vijay...
Chris - Here in the UK, we've managed to reach the milestone of vaccinating 15 million people by the 15th of February, which is about one in four adults in the UK. America, obviously, arguably has quite a long way to go, so do other major territories, but how do you think it's going?
Vijay - I think it's going remarkably well. I think this was such a humongous problem that we were facing. I think the fact that we have developed a vaccine in less than one year where conventional technologies take vaccines to be developed in 20 years is an achievement in itself, okay. These new technologies, as your previous speaker spoke, the messenger RNA and the directed delivery technologies are absolutely amazing because one of the key points in these technologies is they actually take the vaccine manufacturing from a factory into the body itself. They use the body's muscle cell to make the vaccine. So that's a remarkable achievement and we have never used these technologies previously for making vaccines and that's why we were able to achieve this one year roll out of this new vaccine. Yes, we have been a little slow in getting the vaccines out, but the learning curve of experience’s catching up with us. I think you will have plenty of vaccines by the middle of July, middle of this year because there are new vaccines getting approved and the current manufacturers are getting more efficient.
Chris - Our politicians, nevertheless, have said that the limiting factor isn't the will, it isn't the people, it’s the supply of vaccines. Do you see that changing? Because at the moment it does appear that we have sat on our laurels, historically, and we've relied very heavily on supply chains of vaccines coming from remote parts of the world, because we could plan ahead with things like flu vaccines, where there's a predictable annual cycle and we could afford to just ship things in in a just-in-case mentality way and now we need to really rethink that.
Vijay - Yeah, I think so. I think the COVID 19 pandemic is a wake up call. I think we have to rethink our manufacturing strategy for vaccines, for pandemics, even our routine vaccinations. You know, we need to make sure each country has a centre of excellence where manufacturing can be undertaken. I know the UK used to be a Mecca of manufacturing vaccines, and no longer makes any vaccines. GSK is made in Belgium. The same has occurred in Germany, same has occurred in Japan. I think we need to rethink all that, we need to spend a lot of money. But the silver lining is these new technologies - they are less capital-intensive, they're quick, they're fast and they're remarkable. This gives us an opportunity to rethink this whole strategy again and get back to where we once were. We also need, Chris, to get these three big players who are not involved in this COVID-19 vaccine to get on with the program. GSK, Merck and Sanofi are not involved in any of this COVID-19 effort. They have the factories, they have the people, they have the know-how. We need to use government incentives, a carrot and stick approach to get them involved.
Chris - Sanofi have though, under license, been producing Pfizer's vaccine in Europe.
Vijay - They have, but that's a minimal effort. I think they can do more than that. They can do Moderna's vaccine. They have expertise in subunit protein vaccines. They can even do Novavax vaccines. They have those capabilities. They're doing a little bit of things to keep involved but I think they're not really fully aggressively involved as we would like to see. This is a serious issue that has not been talked about. It's the elephant in the room that people have neglected
Chris - That elephant being that if there is COVID anywhere, as Melinda Gates put it, there's COVID everywhere. because we can't just have an I'm all right, Jack mentality. We've basically not solved the problem till we've solved it everywhere for everyone and that means massive scale and that means everyone's got to get behind this.
Vijay - Absolutely, there's got to be global planning. There's got to be global cooperation. You want to make sure you vaccinate people in remote parts of Africa, as well as you vaccinate people in remote parts of the United States and in the UK because you don't want this pathogen to survive in other parts of the world and develop variants, which will eventually, because of a global connected world, going to come back to your own country and haunt you because the vaccines that you're taking now may not be effective against those variants.
Chris - Do you think then that we're going to be looking at some kind of vaccine passport system in future? This has begun to be discussed. People have made various negative noises about data protection and also, as we've been hearing from a couple of our previous contributors this week, we don't actually know what immunity to this thing really means. We don't know how long immunity from vaccination will last. We don't know what immunity to the variants will be. So will it really be meaningful to have some kind of stamp in your passport to say I got vaccinated?
Vijay - I think it is going to become a reality sooner than later. I think the COVID 19 pandemic has taught us that if we were vigilant in the very beginning and we had stopped travel coming out of China, we would have stopped this pandemic in its tracks. And now if a new variant comes in, the only way we're going to prevent it is we're going to have vaccine passports to make sure people are getting vaccinated. And this is nothing new, Chris. This concept has been around for a while. If you want to travel from South Africa to India and if you don't have a Yellow Fever vaccination certificate which is valid, which proves that you had a vaccine in the last two years - if you end up in Mumbai, you'll be put in quarantine if you don't have that passport. It's really strictly enforced and the same thing applies for COVID 19 and the fact that the vaccine may not be effective beyond a year is not the reason not to do it because any vaccine is better than no vaccine.
Chris - The thing is that there are people who will follow the rules. There are also people who notoriously don't follow the rules and it only takes a small cadre of people to bring in a variant, doesn't it, and you've got big land masses, like the US and like Europe, where there are no borders. There are no border posts, there are no checkpoints where people would be asked to prove their immunity status. So there's still enormous potential for the movement of people and therefore the movement of disease. So is it not a hiding to nothing? Is it not just another barrier in the way?
Vijay - No, it is not. I think any control is better than no control. It's like if you live in Cambridge and just because people break into homes, no matter what you do, even if you lock your doors and you take that position that you know what, people break into homes so I'm not going to lock my doors. That's a silly argument. I think we need to put border controls. Yes there's going to be leakage. That leakage is better than a mass movement of people carrying all kinds of variants. So I don't buy the argument that if there's even some backdoor entry of people breaking the rules and getting into countries where they're not supposed to be, that's better than not having this passport control. I think the vaccine passport is an essential thing and it's becoming a reality pretty soon.
Chris - Last point, and this is the hardest question of all, when do you think I'll be able to pick up the telephone and book my holiday abroad, again? How long before we're seeing what we used to call normal back do you think?
Vijay - My guess is way the things are going, how the vaccine rollouts are coming, how vigilant we are, I would say by Spring of next year, I think you should be back on your holiday schedule. You'll be in the Bahamas, if that's what your favourite vacation spot is. As long as you carry a vaccine passport.
Chris - Are you paying Vijay?
Vijay - I'll do my best!
Chris - I'll send you the bill!

54:05 - QotW - Would a foetus develop differently in zero gravity conditions?
QotW - Would a foetus develop differently in zero gravity conditions?
David - Would a foetus develop differently in zero gravity conditions?
Adam M - Making a whole new human being is a complex process at the best of times, even here on Earth. So what would happen to a fetus, trying to develop in space? Adam Watkins is an expert in reproductive biology from the University of Nottingham, and has some insight into why this is such a tricky question...
Adam W - The difficulty in trying to answer this question is that no one has ever fallen pregnant while being in space. Our best understanding of how zero gravity might affect foetal development comes from studies using animals. Initially, rats and mice were sent into space to see how micro-gravity might affect their ability to reproduce. Unfortunately, the significant disruption of travelling into space meant that none of the females who became pregnant stayed pregnant. Astronauts have also studied how embryos from animals such as mice, salamanders and birds develop under lower gravity. Again, these studies showed that micro gravity had a negative effect on the embryos, slowing down their rate of development so that they contained fewer cells than normal.
Adam M - And although since those initial experiments, some animals like rats have given birth in space, the results have been mixed, and of course, a mouse is a far cry from a person. And fully grown people already have enough trouble when they’re in space.
Adam W - In space, astronauts have to take regular exercise to counteract the negative effects that weightlessness has on bone and muscle strength. On earth, a foetus in the womb also exercises, using the resistance of the amniotic fluid to strengthen its bones and muscles. In space, the lack of gravity could affect the development of a foetuses’ bones, muscles and other organs during pregnancy.
Adam M - All of this leads to NASA having a no pregnancy in space policy, and female astronauts are tested regularly before launch to make sure we don’t end up conducting an impromptu experiment on space pregnancy. And that’s not the end of the potential problems
Adam W - Finally, astronauts are exposed to doses of cosmic radiation 100s of times higher than here on Earth. This high-energy radiation can damage our DNA, causing mutations. During a 9 month pregnancy, both the mother and her developing baby could be exposed to harmful amounts of cosmic radiation, which may have unwanted long-term consequences for things like cancer.
Adam M - So as boredchemist said on the forum: it might be prudent to check that idea with something bigger than a mouse before we risk a human.
Thanks to Adam for delivering that answer, next week, we’re getting our teeth into this one, from James
James - What were the health impacts of the vastly different diets and lifestyles of aristocrats and peasants? Would wealthy Roman patricians be much smarter than plebeians based solely on improved nutrition?










Comments
Add a comment