40 years since the identification of HIV, we look at where it came from, and how far are we from an effective vaccine…
In this episode

00:43 - Where did HIV come from?
Where did HIV come from?
Paul Sharp, University of Edinburgh
This week, we’re marking 40 years since the identification of a virus responsible for an estimated 40 million deaths: HIV. Will Tingle has been looking back at the timeline…
Will - June 5th, 1981 - the CDC publishes a paper reporting a rare form of lung infection in five young, previously healthy gay men in Los Angeles. And for some reason, their immune system is no longer working properly either. All five will die. The same day, a dermatologist calls the CDC to report a cluster of cases of a rare and unusually aggressive cancer among gay men in New York and California.
Anthony Fauci - We were calling it 'gay related immunodeficiency' or 'the gay cancer'. Because of Kaposi's sarcoma.
Will - The mysterious disease spreads throughout the gay community. The fact that this disease destroys people's immune system leads to it being named 'acquired immune deficiency syndrome' or AIDS, but the underlying cause is still unclear.
TV Interview - I had noticed these bumps on my skin and they looked a little suspicious. Uh, they didn't hurt, but they were very strange and they were multiplying.
Will - By the end of 1982, the number of confirmed deaths in the US reaches over 1000 and it is spreading fast.
TV Interview - Well, I think it's definitely transmissible, uh, just how, I don't know. Is it through blood? Uh, is it through saliva? Is it through... I don't know.
News Report - Paris today. Shocking figures about a deadly disease. 90% of those infected don't realise they've got it.
Will - May 20th, 1983. Finally, a breakthrough. Dr. Françoise Barré-Sinoussi and her colleagues at the Pasteur Institute report the discovery of a retrovirus that could be the cause of AIDS. That retrovirus is HIV. Her theory is later proved right, and she will win a Nobel Prize for it in 2008. So we've had the name for HIV for the past 40 years, but the virus itself has existed far longer than that.
Chris - Indeed, so where did this virus originate? And how? Paul Sharp, geneticist at the University of Edinburgh has spent much of his career following this detective story. The clues point to a jump of a related virus called SIV carried by chimpanzees into humans, most probably in the environs of Kinshasa, the capital of the Democratic Republic of the Congo. But when did this happen, and how do we know?
Paul - It's probably at least a hundred years ago. What we think is that one virus initially emerged in humans. And from that, as it spread through the human population, it has accumulated mutations in its genome and those changes occur at a fairly steady rate. So given that we now understand how fast those changes occur, we can look at the difference between two strains and ask when their common ancestry existed. And so we would estimate that they started to diverge about a hundred years ago.
Chris - And geographically, where was all this going on?
Paul - Well, we can see today that the greatest diversity of strains of these viruses is in the area around Kinshasa. And that suggests that that's where the virus really first started to diversify into these different forms. But we also can trace where the virus likely jumped first into humans because we have looked at samples from other primates that have a virus very closely related to HIV1.
Chris - Ah, so your argument is that some other animal, probably a primate, had a virus very similar to HIV, which got into humans and became HIV, sort of similar to how a bat virus that's a coronavirus can jump the species barrier and cause COVID-19 in us.
Paul - That's right. So when HIV1 was first discovered and described, the only virus that was known that was closely related to that to human virus was one which is found in sheep. But very quickly, people started to discover more closely related viruses in non-human primates, in monkeys and in apes in Africa. And so by about 1990, we knew of several different monkey species, which had these viruses, the viruses in the non-human primates, called SIV for simian immunodeficiency virus. The virus in non-human primates that was most closely related to the human virus was the one found in chimpanzees.
Chris - So how did it get from the chimps into us?
Paul - We can't know because this is probably something that happened more than a hundred years ago. So we can only speculate about what is likely to have happened. We know that HIV can be transmitted amongst humans through blood, and we know that humans in West Central Africa where we think this happened, hunt chimpanzees. And so when you hunt a chimpanzee, you are likely to do some butchery immediately that you've killed in order to carry it away more easily. And at that point, there would be blood with the chimpanzee virus in it, which could easily spread to an open wound on the hunter. And so we think that it's most likely through the butchery of chimpanzees that this virus spread into humans.
Chris - Presumably these viruses have existed in the primate species for hundreds to thousands of years and people have been hunting them for hundreds to thousands of years. So why did this happen when it did?
Paul - What we think changed was humans. In the sense that in this part of West Central Africa where we think the transmission from a chimpanzee to a human first occurred, until about a hundred years ago there were no really big settlements. There were no cities as such in West Central Africa. And it's only a little over a hundred years ago that people started to gather together in large congregations in large cities. And what we suspect is that the virus which would've initially been transmitted to an individual in a rural area would've needed to get to a large city, a large collection of people, for it to actually really take off in initially an epidemic, which became the pandemic.
Chris - Can I draw you then on where specifically you think all this was going on?
Paul - Chimpanzees, the common chimpanzee, actually is divided into four different subspecies, and only two of those subspecies are infected with the virus that is the ancestor of HIV. So chimpanzee viruses from one specific area, which is in the very southeast corner of Cameroon. These were the viruses that were specifically close to HIV one. And it indicated to us that this was the part of the world where the jump to a human first taking place. That's a very isolated rural area. I mentioned that the virus probably had to spread to a larger city in order for it to really get going. So what we can see when we look at the map is that the part of Cameroon where the chimpanzee viruses are, is surrounded by rivers which all flow south and join into the Congo, which then of course flows past Kinshasa. So the virus has made its way through one more series of infected individuals to Kinshasa. There it has started to really spread among people, and then it has spread out from there. And what we see then is, in the genetic makeup of the virus, we can see different strains of the virus that have spread to different parts of Africa. And then having spread across Africa, they then spread out across the world. One of my colleagues has shown that the most likely route out of Africa initially was through the Caribbean, through Haiti and then from Haiti into the United States, from the United States over to Europe.
Chris - That's quite a journey, isn't it? So that there was a huge sort of iceberg here. This was drifting on for maybe a century, nearly a century before we realised that it was established in all these different populations, in all these different geographies.
Paul - I'm often asked how could it be possible that a virus as deadly as HIV could be present in the human population for 50 or more years without us knowing about it. And the answer is, I think, fairly straightforward. If you look at the idea of, say, an exponential spread of a virus from one or a few people being infected a little over a hundred years ago to the many millions that have been infected now. If you chart the, the rate of increase in numbers are infected individuals, you would speculate that only a few thousand people had been infected by about 1960. And those people would all be in Central Africa and they would be, when they got ill from AIDS, they would be suffering from a wide variety of different disorders. Because what the AIDS virus does obviously is destroy your immune system and make you susceptible to other infections, other bacterial or fungal infections. And so it doesn't surprise me at all that this virus could go under the radar for such a long period of time.

10:15 - Who is most at risk from HIV today?
Who is most at risk from HIV today?
Annie Howard, National Aids Trust
So now that we understand the origins of HIV, what has happened since then? Every disease outbreak affects certain groups more than others, so which demographics are most at risk? Annie Howard is from the National AIDS Trust...
Annie - At the end of 2021, which is the most recent year that we have accurate data for, the World Health Organization reported that there were 1.5 million new cases of HIV globally, which would equate to over 4,000 per day, which is far too many, considering that we now have effective treatment and prevention mechanisms to manage an epidemic.
Chris - How many people around the world right now then do we think are currently living with this infection?
Annie - So we estimate it to be around 35 million. Again, that was in 2021, so probably more now. But what I will say is that while that is a high number and actually is the highest number that it's ever been, this is kind of attributed to two different things. So of course, in part, that will be attributable to new HIV cases, which we want to stop as the ultimate goal, and 2030 is the global goal to stop new transmissions, and new cases have reduced by roughly half since the peak of the epidemic in 1996. But the other part of that large number is that a large number of people living with HIV are now doing so thanks to these effective treatments that we have, which allow them to live full and healthy lives as anyone else would. So this is really important to reduce the viral load of HIV within the individual. And in the field we use the term ‘U=U’, so undetectable equals untransmissable. So the more individuals we have on effective treatment, the less transmissions that we're going to see, and then we'll really reduce that number. So the fact that there are less people getting really sick and dying from HIV means that more people are living with it. So that large number isn't actually all really bad.
Chris - Where are most of these cases?
Annie - It's really variable across the world. So the African region continues to be the most severely affected. So that region accounts for around two thirds of the global cases. Different countries need different interventions to really target those different needs. And obviously, low and middle income countries are experiencing different social environments. So the needs there would be quite different to say what we see in the UK.
Chris - Indeed. Who do you think are the most vulnerable communities that we need to keep our eye on in terms of preventing increases and making sure we meet those goals of stopping transmission by 2030?
Annie - So a lot of the work we do at the National AIDS Trust in partnership with the European Center for Disease Control focuses on the European region. So I can mostly speak to that. And the groups in this region are mostly men who have sex with men, which is probably the group that people most align with this disease. But also people who inject drugs, sex workers, migrants, prisoners, and heterosexual women are all groups that we need to be really focusing on.

14:10 - What HIV does to us, and how we treat it
What HIV does to us, and how we treat it
Jordan Skittrall, University of Cambridge
What happens inside the body when infection occurs, and how do the drugs we now have combat the virus? The University of Cambridge's virologist, Jordan Skittrall…
Jordan - There are three main ways HIV can get into the body. The most common is by sex. It's usually sexually transmitted. It can be transmitted directly from one person's bloodstream to another, if they come into contact in some way. That can be via blood transfusion or by injury. And the third way is that it can be transmitted from mother to baby. So vertically.
Will - Once HIV is inside the person's body, where's the first place it heads towards?
Jordan - HIV infects a number of cells, mostly cells that circulate around the blood. The most important of these eventually is a class of white blood cells that we call T cells. What it does is it goes into those cells and archives a copy of itself in the genetic material of those cells.
Will - What's the plan then? What's it trying to do?
Jordan - It does two things from that point. One is it then uses the cells own replication machinery to make copies of itself that then come out and go on to impact other cells. But not all of the HIV does that. Some of it becomes archived within these cells. So some of these cells form part of the immune system that provides our immune memory and our bodies are set up to keep a stock of those cells in the archive so that when we respond to new infections, we have the memory available. So HIV can use the body's own way of keeping that record alive to keep itself working.
Will - What does HIV do once it has gained the ability to self replicate within our T cells?
Jordan - It just keeps on infecting more and more of those blood cells without any intervention. This is where it can get slightly confusing because it's possible for the immune system to react against that, against infection of the immune system. But a lot of the disease you see from HIV in late infection is as a result of the immune response taking out some of your own immune system and there's this sort of tug of war back and forth between making more of the cells to keep your immune system functioning and HIV infecting them. So that can carry on for a while until late on in infection where the HIV is beginning to win the tug of war, as it were, so that there are fewer and fewer of those T cells to in fact the white cells to infect.
Will - If HIV is effectively decimating our white blood cell count, our body's immune response, that must mean that the body is severely immunocompromised. Is that the case then? Does the problem become other infections and diseases in our body that previously we wouldn't even have blinked at are suddenly much more problematic?
Jordan - Exactly. So some of these things are infections that we don't even know about. We probably didn't even notice when we got them in the first place. They just live happily with us and we keep them under control. Sometimes they are environmental infections, so things that might just be wafting around on the breeze that have come out of the soil. But again, we normally just keep it under control.
Will - Presumably then with all these stages involved in the infection, we've got a lot of stopgaps that allow us to sort of chuck in an inhibitor or a drug that stops the virus from working at a certain stage.
Jordan - So there are a couple of classes of drugs that will act against HIV when it's trying to enter the cell. Some very important classes of drugs that stop HIV making copies of itself to integrate into the host genome. We have drugs that stop that integration step and we also have drugs that stop the final preparation of the proteins within the virus particle.
Will - Presumably then why throw one of these at the problem when we can throw all of them at the problem?
Jordan - We tend to throw two or three of them at a problem usually when we see somebody. And the reason for that is HIV mutates really rapidly. In somebody who's infected with HIV, there's an entire population of just slightly different versions of the virus. And if the virus is being exposed to a drug but not being completely suppressed, then it is possible for some of those mutated virus to get around single drugs. So what we do is we give the drugs in combination so that the virus cannot overall get round the lot of them, which means that we can keep it under control.
Will - Now as with any virus, HIV can mutate. Is that why HIV is so difficult for the body to find and could it even be a problem for treatment drugs as well?
Jordan - The main problem isn't so much that HIV can mutate around immune response, although it does do that, but the immune system can respond in kind. The problem is, because it's archived itself within the cells, some of which are being maintained as a population for decades, if not the entirety of someone's life. The difficulty is that when it's just sitting there within the DNA in someone's cell and not making a new virus, there's nothing to see for the immune system. So even though you can respond to the cells of the making active virus, there's still this reservoir of cells that are sitting there just waiting for their moment to start replicating at which point you might be seeing virus coming out again.
Will - And that's why, for all the wonders that this treatment does, it's not a cure because if you stop taking these drugs three weeks later, suddenly it's back.
Jordan - Yeah, exactly. It's a really effective treatment and it can keep the virus under control for the entirety of someone's life, but you have to keep taking the pills.
20:35 - New HIV vaccine enters human trials
New HIV vaccine enters human trials
Julie McElrath, Fred Hutchinson Cancer Centre
Almost exactly 40 years ago, Parisian researchers Luc Montagnier and Francoise Barre-Sinoussi, announced that they had isolated the virus responsible for causing AIDS; they called it HIV - human immunodeficiency virus. In the wake of the discovery, which earned the pair a Nobel Prize, a bullish medical community predicted a vaccine within a few years. Yet 4 decades on, we're still waiting.
The evidence that it should be possible to make a vaccine is that if we look at people who have been infected with HIV for a year or so, often they make very powerful antibodies capable of stopping HIV - in all its different forms - in its tracks. By then, of course, for them it's too late, because the infection has already taken hold throughout the body. But if those antibodies could be produced by a vaccine before a person was infected, then they should be well protected.
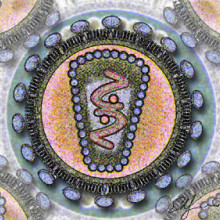
The problem has been engineering a vaccine capable of making the immune system respond in the right way to do this. You need to show the body the right part of the virus in the right way to make the immune helper T cells cooperate with the antibody-producing B cells to generate high levels of antibodies. The virus has naturally evolved to thwart this process, and keeps the parts of its outer coat, or envelope, hidden from the immune system to reduce the chances of this happening. And that's why vaccines have been hard to make.
But now, Julie McElrath, at the Fred Hutchinson Cancer Centre in Washington, has developed a new way to do it: she's got what can best be described as a “molecular meatball” comprising a particle that has sticking out from its surface multiple copies of the linchpin part of the viral coat that she wants the immune system to react against. Because this effectively force feeds the immune system with the region of the virus that HIV normally strives to keep hidden, it provokes a strong response, which she's recently been able to test in human clinical trials…
Julie - So the vaccine is a particle and that particle is displaying a part of the HIV envelope, but in multiple copies, up to 60 different copies of it. By having all those copies and the fact that they're displayed in a way that it's going to ignite that really early process is key. So we're showing it the right thing. And then also the molecule that allows that to be held together as particle is also being seen. And so that also stimulates the T cell response as well. All of those factors help to get a really strong T cell response that can be pretty broad, and that way we can nurture the B cells in the way that they need to be nurtured in order to eventually mature into the response that we need.
Chris - So how have you tested this so far and what gives you confidence that you're on the right track?
Julie - So we've given the vaccine to healthy adults in two doses, two months apart, and blood is drawn before they get any vaccine and then it's drawn after they get each dose of the vaccine. And so we're looking for what is new, what has been induced by the vaccination. And so we can look at the B cells, we can look at the T cells, and we look at the antibody responses. And it's from looking at all three of those things that we can understand how the vaccine is working in particular for the T cells, we're looking to see what they're recognising and they're recognising the parts of the vaccine. The B cells are being activated by parts of the vaccine to make these antibodies that can recognise and important targets to neutralise an incoming virus.
Chris - Can you take samples of those antibodies from those human recipients and demonstrate that they're capable of neutralising the virus for real? Can you do tests like that to then prove those antibodies are capable of knocking the virus on the head where an incoming infection in those people?
Julie - We can do that. That's part of what is done in these studies. So you basically look to see, well, how does it do it? Can it block infection? So those are the types of experiments that have been done to determine what the response is in these vaccine studies.
Chris - HIV is notoriously slippery as a target. It's a shapeshifter, it continues to evolve and change its appearance. So what makes you think that the antibodies that you are making here to this vaccine will continue to protect against strains of the virus that are continuing to evolve in a population?
Julie - Yeah, with this vaccine, we're going after just one part of the envelope that we know is a target for neutralisation, but there are others, seven or eight of them. So it's very likely that we'll need to look at additional targets other than this one. But this is a start. Starting with one, which we think is a really important target. And then we'll be looking at other places on the envelope in a sort of similar way to try to attack that. Ultimately the vaccine that we come up with will likely have to target more than one site.
Chris - Wouldn't it be nice if this year, 40 years after Françoise Barré-Sinoussi, from the Institut Pasteur in Paris said, we know what the virus is that's causing this and we'll have a vaccine in no time. And that was 40 years ago. Wouldn't it be nice if on the 40th anniversary you do get this to work? Are you now going to move this in a phase two trial where you're actually going to see if vaccinating a susceptible group of people does lead to protection?
Julie - So the things that are in process now is to test this in the form of an mRNA, similar to that platform that's been used in COVID. And so we're looking at that because as you know, the mRNA technology allows us to move fast. They can be made quickly. And so that's happening. And then the other thing that is happening is we have to boost this response. So it's going to be a sequential vaccine approach. And so we're now looking at the second step, the booster.










Comments
Add a comment